“Rainbow baby” Olivia Landry: A journey of hope through the NICU
- Category: Patient Stories
- Posted on:

Kandi and Chris Landry were overjoyed to celebrate their daughter Olivia’s first birthday, filled with love and laughter, especially after the challenging first year she endured.
They were enjoying life with their son, Ryan, now 9 years old, but were looking to expand their family. After the heartbreak of losing their second son to stillbirth, Kandi and Chris were uncertain if they would ever experience the joy of pregnancy again. However, after one round of IVF, they were excited to find out they were pregnant with their first baby girl.
In the fall of 2022, Kandi’s water broke when she was just 14-weeks pregnant. “I was told nothing could be done. They said they didn’t think she would survive,” Kandi recalled. “But we wanted her so badly. Her heart was beating, and we decided to do everything we could to give her the best chance at life.” 
Kandi wasn’t admitted to her local hospital for bed rest until 10 weeks later. Finally, at the 24-week mark, doctors decided to intervene to improve the baby’s chances of survival. However, with little to no amniotic fluid protecting her, they cautioned that Olivia’s chances were still slim.
At 28 weeks, Kandi went into premature labor on February 19, 2023, and Olivia was delivered by emergency Cesarean section. She weighed 2 pounds, 8 ounces, and was a tiny 13 inches long. The first week of her life, Olivia battled underdeveloped lungs and a pneumothorax that wasn’t healing properly in their local NICU.
“Every day, they had me thinking ‘today would be her last day.’ It was such a horrible feeling,” Kandi said. “They just couldn’t handle Olivia’s lung issues.”
Knowing that Olivia needed specialty care, Chris and Kandi made the decision with their doctors to airlift Olivia to Children’s Hospital New Orleans. Chris admitted how scared they were at the time. “It was terrifying to learn that they couldn’t care for Olivia and that her condition was so severe that she needed to be taken to another hospital to get the proper care,” he said.
When the couple arrived at the Children’s Hospital New Orleans designated Level 4 Neonatal Intensive Care Unit (NICU), the neonatology team had already assessed Olivia and had a plan to treat her.
That’s when everything changed for the Landry family. “As soon as we got to CHNOLA, we were immediately given hope,” Kandi said. “We were told that she was going to grow, her lungs would grow and she was going to be OK. I was still worried but I absolutely felt a sense of relief after meeting neonatologist Dr. (Michelle) Knecht. Finally, we were confident Olivia would get the care she needed.”
Olivia stayed in the NICU at Children’s for 200 days. The family prioritized being by Olivia’s side as much as they could while balancing school and work. Every day, Kandi would drop her son off at school in Mississippi, and then make the long drive to New Orleans to be by Olivia’s side. A few hours later, she would kiss Olivia goodbye and drive back to retrieve Ryan from school.
Chris, a lineman, would visit his baby girl two days a week when he was off work.
“It really was a waiting game,” Kandi said. “Our NICU stay was relatively quiet. We were waiting for Olivia’s lungs to grow and catch up to the rest of her body. They were always monitoring vent and oxygen settings. Dr. Knecht and the team took such great care of her.”
Dr. Knecht was the first doctor the family met at Children's Hospital New Orleans and was there for a lot of Olivia’s pivotal moments. “Once Olivia was more medically stable, Dr. Knecht took her outside for fresh air for the first time in her life,” Kandi remembered. “We were nervous about it, but Dr. Knecht reassured us. She put Olivia in a wagon with the necessary medical equipment and we went outside for our first family outing.” 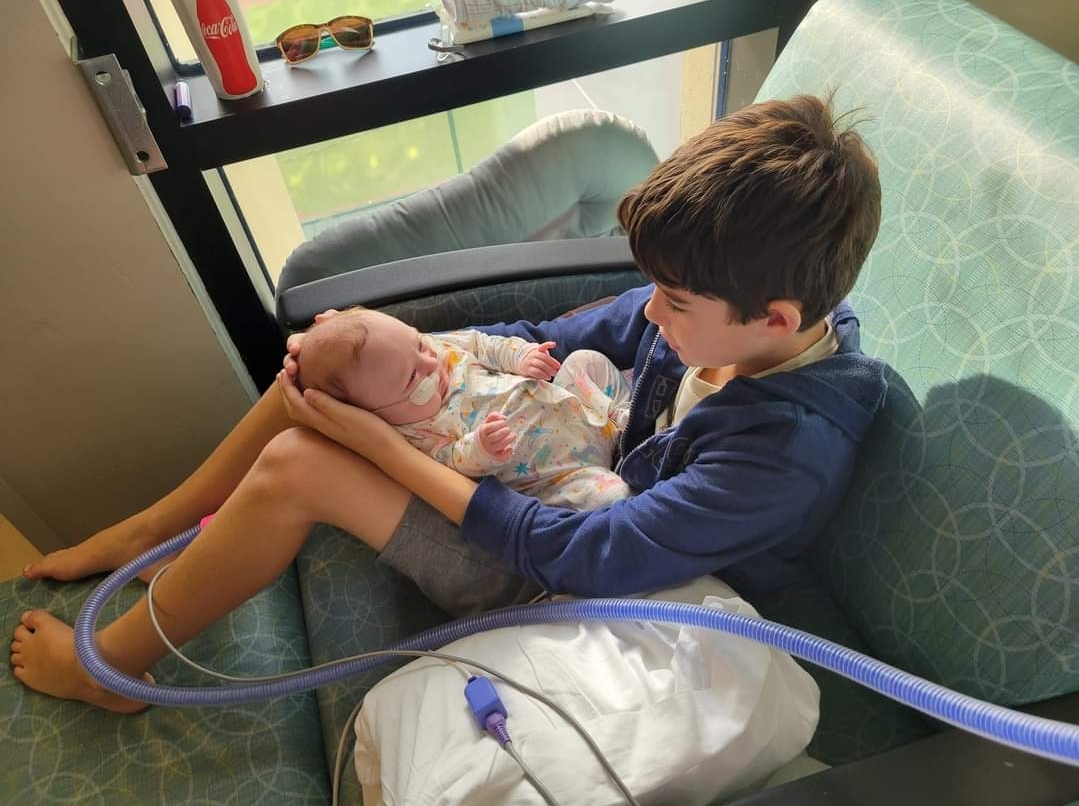
When discussions about inserting a tracheostomy (trach) started, the parents were very nervous. “Dr. Knecht explained things in a way that made us understand things,” Kandi said.
“Hearing your child needs a trach was alarming,” Chris added. “No one is used to seeing that on a baby. We think of trachs as something older people or longtime smokers need. This was my little girl.”
However, with the guidance of Dr. Knecht and another neonatologist at Children’s Hospital New Orleans, Dr. Jeffrey Surcouf, the couple came to realize just how crucial the trach was for Olivia’s growth and her eventual discharge from the NICU.
Kandi and Chris praised the many members of their care team for their expertise and support during this vulnerable time. “Dr. Surcouf held some meetings between us and his team and that made all the difference,” Chris said. One of the respiratory therapists, Shauna, also helped the couple feel at ease. She trained them on how to care for the trach. “We felt confident and ready to take Olivia home, thanks to Shauna,” Kandi said.
Kandi expressed her deep gratitude for the doctors, nurses, and physical therapists at Children's Hospital New Orleans, saying she could never thank them enough. The couple especially appreciated NICU nurses like Hannah Guidry, who had a sweet and calming presence that made them feel comfortable leaving their baby in her care. "We could tell how much she truly cared," Kandi shared. "In fact, I often felt like they were taking care of me just as much as they were caring for Olivia. I may not remember all their names, but the nurses there are simply wonderful."
Olivia was discharged five weeks after her trach was placed on September 7, 2023. That’s when the family was able to start their lives with their new baby girl at home. Olivia needed a portable ventilator for a long time, and Kandi and Chris were happy to “lug” the equipment along if it meant they could enjoy family time outside the house. 
More recently, she is only attached to the equipment at night. Olivia receives follow-up care with pulmonologist David Swetland, MD, every three months. “I like how he goes at Olivia’s pace. He is very calm about everything and was supportive of my interest in starting to get her off the vent and showed me how to do that. He taught us how to see if she was struggling. Dr. Swetland is wonderful,” Kandi said.
Some more tests will soon determine if the baby can stop using the vent and Kandi is hoping the trach will be removed by this time in 2025.
Nothing, not even the equipment helping her breathe, can stop Olivia from being on the move. She is sitting, standing up and trying to crawl. She gets closer to walking every day. “Just try to slow her down when she is in her walker,” Kandi said.
“Her brother is her favorite person in the whole world. Olivia lights up when she sees him! No one can get her to laugh the way he can.”
Chris said Children’s Hospital New Orleans makes long term care so easy. “I love that they condense all of Olivia’s doctors’ visits into one day. Instead of having many appointments and having to drive back and forth, we sit in one room and all her doctors come to see us. In two, three hours, you’ve seen every doctor you need to see. That’s truly amazing. We don’t have to carry around all her equipment and visit several buildings. It makes it so much easier on us as parents. I love that about Children’s.” 
When Kandi recalled the day her water broke in the fall of 2022, her eyes welled up with tears. “Olivia was our rainbow baby. It was supposed to go better this time. But finding out she may not survive was more than devastating. Now it’s well over a year later. I’ve found out that when people tell you to enjoy every minute, you should. It goes by so fast.”
Now, Kandi and Chris are looking forward to a happy, healthy future. “All we want is for Olivia to be a happy kid,” mom said. “It’s our biggest wish. She has been through so much in her short life. She deserves a lifetime of health and happiness going forward.”
To learn more about the Pulmonology program at Children’s Hospital New Orleans, please visit: https://www.chnola.org/services/pulmonology/.
To learn more about the Neonatology program at Children’s Hospital New Orleans, please visit: https://www.chnola.org/services/critical-care/neonatal-intensive-care/



